(update 3/23/2020)
This article covers
1. Are viruses alive?
A virus is a biological particle that can only reproduce inside the cells of living hosts. Based on biologist’s current definition of “Life”, viruses are not living organisms. It is mainly because viruses cannot live by themselves. They need hosts to be live and to propagate.
A virus consists of two or three parts:
- genes, made from either DNA or RNA (genetic materials);
- a protein coat that protects the genes;
- a lipid envelope in some viruses.
Over 5,000 species of viruses have been discovered. Some of them can cause diseases if a person is infected, for example, flu by the influenza virus or COVID-19 by the novel coronavirus.
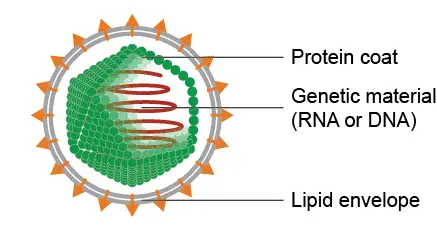
The basic structure of a virus. You can see the virus does not have any organelles and can’t produce the energy by itself. The viruses rely on the host cells to do all kinds of biological activity for them. Image modified from the work of Anderson Brito.
2. What is COVID-19?
COVID-19 means “coronavirus disease 2019”. COVID-19 is caused by a novel coronavirus (2019-nCoV) that has not been previously identified.
Coronaviruses are a family of viruses that share the same features: they all have spike proteins on the surface of their viral particles. This is where the name “corona” viruses came from because they look like crowns. Coronaviruses have RNA as their genetic materials. Some types of coronaviruses frequently cause the common cold and they are not very harmful. However, the novel 2019-nCoV viruses are totally new to us and so no one has immunity to defend them.
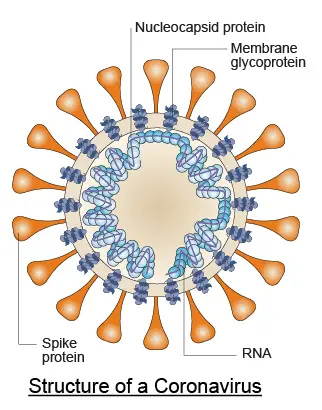
Structure of a coronavirus. Modified from Nature Reviews Microbiology volume 2, pages602–607(2004).
3. Why are people so afraid of COVID-19?
COVID-19 is a respiratory illness that can spread from person to person. We are so afraid of these new viruses because no one had ever encountered them nor had immunity to defend them. Drug treatments and vaccines are not available at this time and may need time (3 months to one year) to develop and test.
In addition, these viruses spread quickly between peoples. Scientists use the term “R0” (or basic reproduction number) to measure their ability to spread. In brief, R0 is the average number of people who will catch the disease from a single infected person. R0 of 2019-nCov is estimated to be between 2-3, meaning one infected person can spread the viruses to 2-3 people. This is why we see an exponential increase of infected patients.
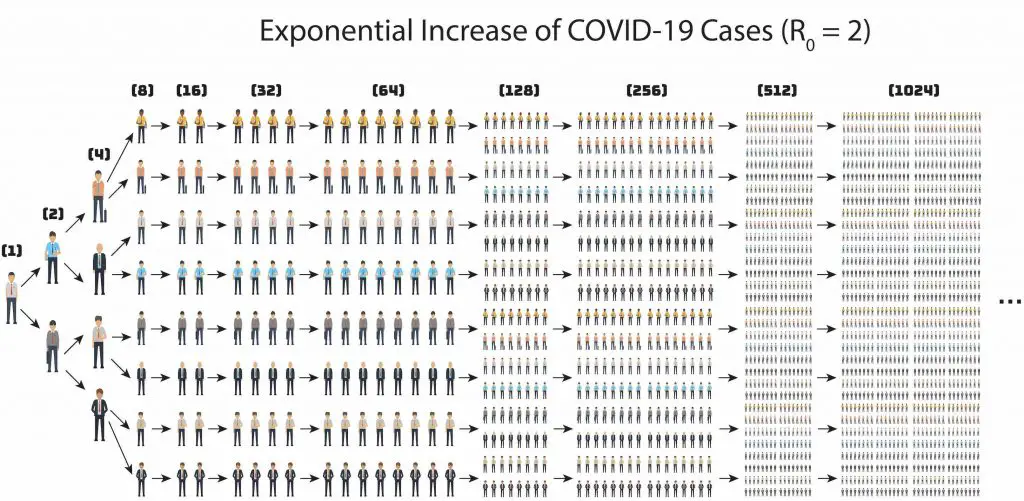
When R0 is equal to 2, it means that a single infected person can spread the disease to two people. If the spreading is not under control, the number of infected people will grow exponentially.
Another scary thing about this sneaky 2019-nCov: some of the patients do not have symptoms or very mild conditions just like normal flu, so people are not aware of getting infected. They continue to hang out with friends and spread the viruses to friends and families. That why we need to practice social distancing.
4. Can someone spread the virus without being sick?
Yes. Most patients who are young and healthy have a relatively mild symptom of COVID-19 while older adults and people who have serious underlying medical conditions like heart disease, diabetes, lung disease become much severe.
Patients with mild or no symptoms (asymptomatic carriers) can still spread their viruses. Sometimes, they do not even notice they are infected because the incubation time of the COVID-19 could be 1-14 days. This makes COVID-19 very difficult to contain.
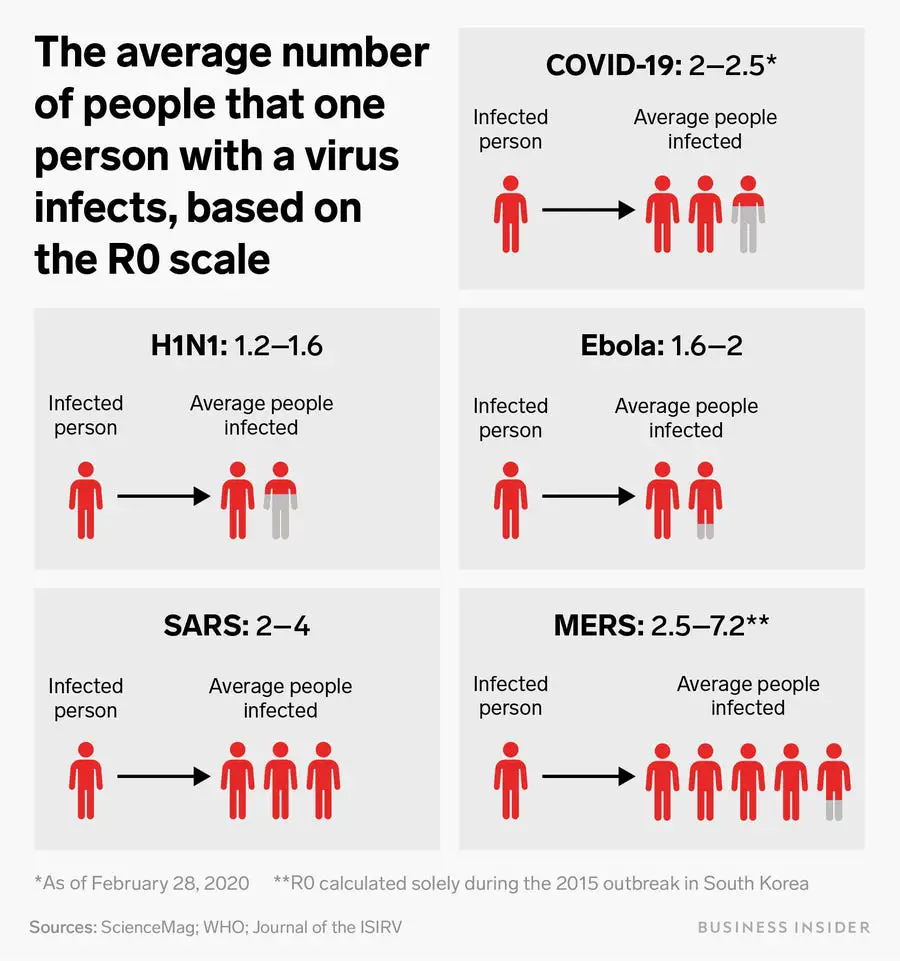
Some other viruses (like SARS and MERS) may have higher R0 than 2019-nCoV. However, patients with SARS or MERS have obvious symptoms (fever). This allows us easily to screen for the virus carriers and prevent spreading. On the other hand, many carriers of COVID-19 are mild or no symptoms. This makes COVID-19 very difficult to contain.
5. How does COVID-19 spread and transmit?
This virus is thought to spread mainly from person-to-person. When an infected person coughs or sneezes, these viruses travel through the respiratory droplets. These droplets can land on the mouths or noses of people who are nearby or possibly be inhaled into the lungs. Another possibility is that these droplets can land on other surfaces and viruses can keep their ability of infection for several hours. It may be possible that a person can get COVID-19 by touching a surface or object that has the virus on it and then touching their own mouth, nose, or possibly their eyes.
Some people hope that once the temperature is getting warmer, the spreading of COVID-19 can slow down. This is because most viruses are sensitive to heat. However, we can not predict this is true for COVID-19 because we still know very little about it.

6. What happens when COVID-19 enter the human body?
Once the viruses are inhaled into the lungs, they will find a way to invade the lung cells. Scientists found that the spike (S) proteins on the surface of viral particles bind to a human cell membrane protein called angiotensin-converting enzyme 2 (ACE2) to enter human cells.
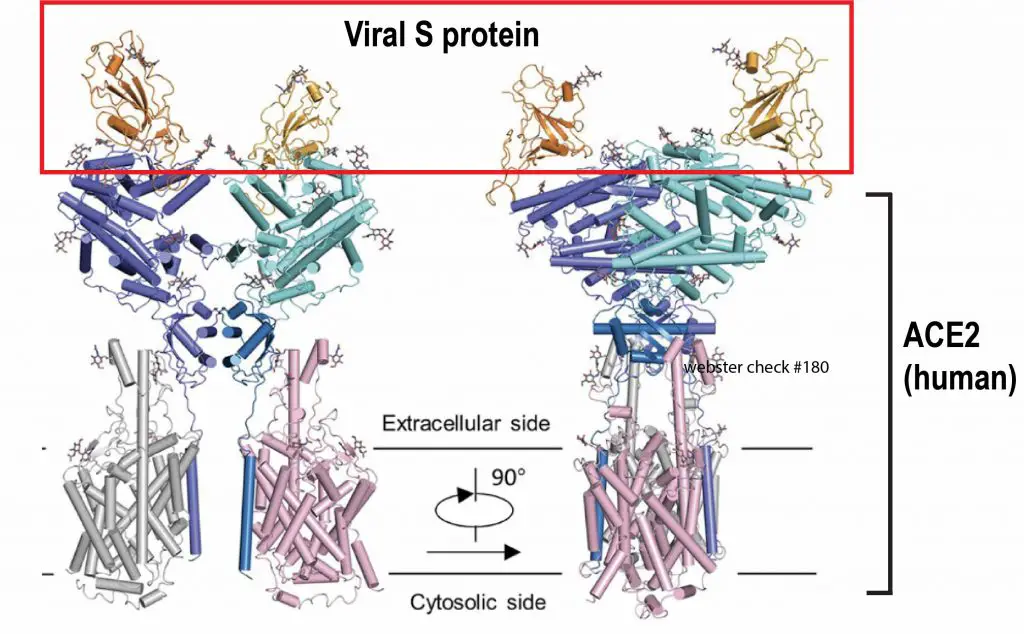
Scientists used the cryogenic electron microscopy (cryo-EM) to study how viral S protein binds to ACE2 on host cells. Cryo-EM is an advanced electron microscopy technique to look at the molecular structure in an extremely cool environment. Cryo-EM allows us to see a biological molecule at a near-atomic resolution. In 2017, the Nobel Prize in Chemistry was awarded to three scientists for developing cryo-EM. Now, cryo-EM proves its value on acquiring this critical information of how COVID-19 viruses infect host cells. This saves a lot of time for scientists to design drug treatments for COVID-19. The Image modifier from Science (2020) Mar 4. pii: eabb2762.
Through the mediator ACE2, the viruses then fuse with host cells and release their RNA genetic materials into the cytosols. The viruses hijack the host cells to produce more viral proteins and replicate more viral RNA, resulting in more new viruses. These new viruses will escape from the host cells and infect more healthy cells in the lung or spread out through coughing and sneezing.
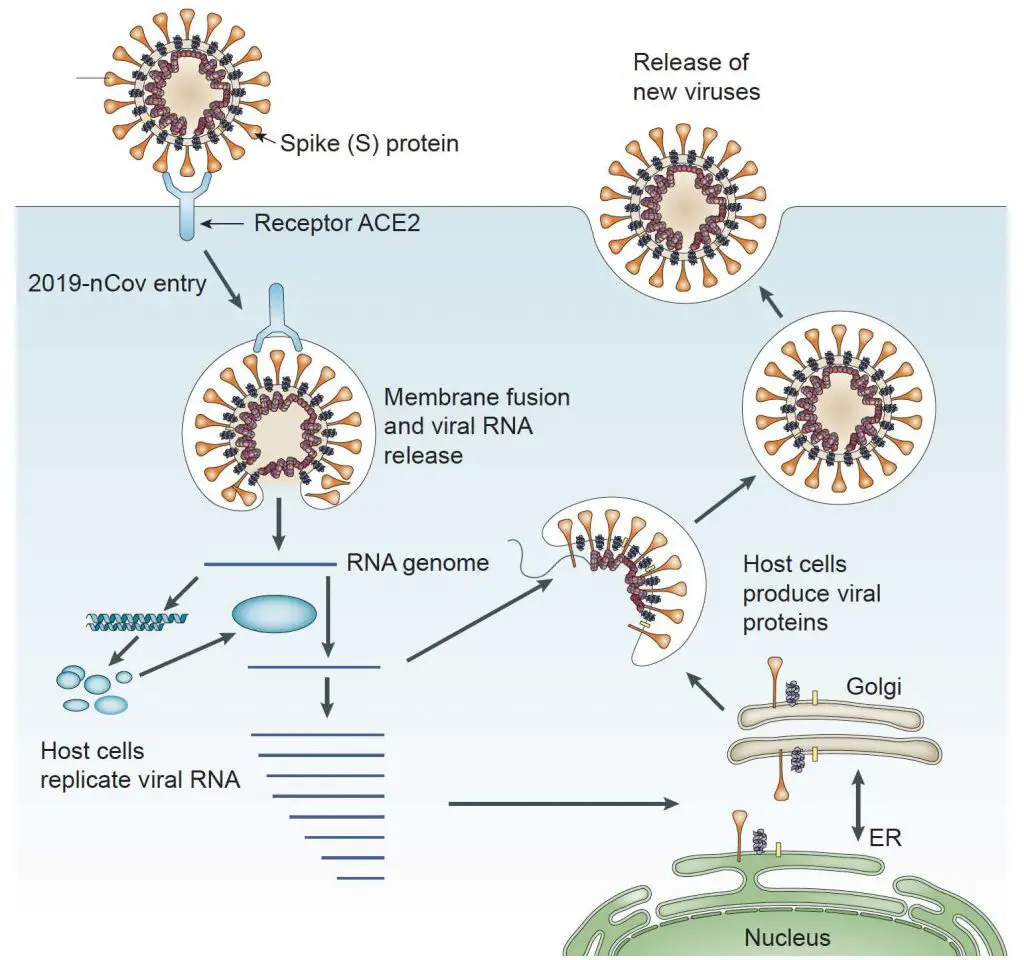
Modified from Nature Reviews Microbiology volume 7, pages226–236(2009)
7. How does COVID-19 kill sick patients?
Once inside the body, the coronavirus invades the host cells that line and protect the respiratory tract. When the viruses reproduce in the host cells, viruses also cause the damages of host cells. Since the viruses hijack the cells to work for virus reproduction, these cells can not perform their normal function. More seriously, the host cells will burst when many new viruses release from the host cells and eventually die.
At the same time, our body will try to fight the viruses by the immune response. Various white blood cells will gather and produce several proteins trying to contain the infection. However, the body’s effort to heal itself may be too robust, leading to the destruction of not only virus-infected cells but also healthy tissue. Overall, the virus infection causes severe damage to the airway and lung tissue. In clinical, we call this pneumonia.
8. Why do people have hope on Remdesivir?
Remdesivir, developed by Gilead Sciences Inc., is an antiviral drug that was originally designed for Ebola virus disease. Remdesivir blocks an enzyme that viruses need for their RNA replication. Since COVID-19 viruses also have RNA as their genetic materials, Remdesivir may stop the virus replication and treat COVID-19. Remdesivir is being used in the first clinical trial of an experimental treatment for COVID-19 in the USA. However, the result is not published yet (March 2020).
Since HIV is also an RNA virus, several drugs that were developed for AIDS may also have the potential to treat COVID-19. Let’s hope the scientists can reveal good news soon about the progress of COVID-19 treatments.
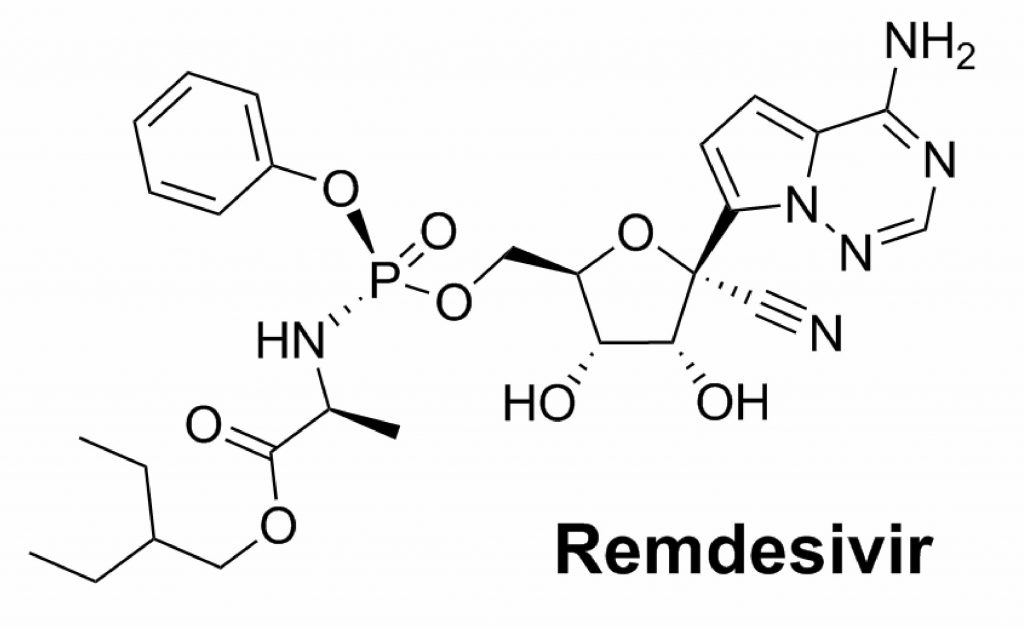
The chemical structure of Remdesivir. Source: https://commons.wikimedia.org/wiki/File:Remdesivir.svg
9. How does our immune system defend COVID-19?
Our immune system has a general and fast response “Innate immunity” to defend a viral infection. The immune system can produce proteins such as interferons to stop virus entry. One type of immune cells, called natural killer cells can be activated to kill the infected cells directly.
However, a more effective defense of COVID-19 requires our body to develop the “Adaptive immunity”. This process will take a few days to 2 weeks and it needs collaboration between several types of human white blood cells. Among them, B cells can release special proteins called antibodies that can bind and neutralize viruses with high affinity. On the other hand, T cells can recognize and kill the infected cells to stop further virus reproduction.
The power of Adaptive immunity is that once we recover from our first viral infection, we acquire the memory of this particular pathogen. If we encounter the same viruses again, our body can immediately respond to it by the massive production of antibodies against the same viruses.
10. When will we have a vaccine for COVID-19?
A vaccine can allow us to acquire the Adaptive immunity to a particular infectious disease without being actually infected by the pathogen. A vaccine typically contains an agent that resembles a disease-causing microorganism and is often made from weakened or killed forms of the microbe, its toxins, or one of its surface proteins.
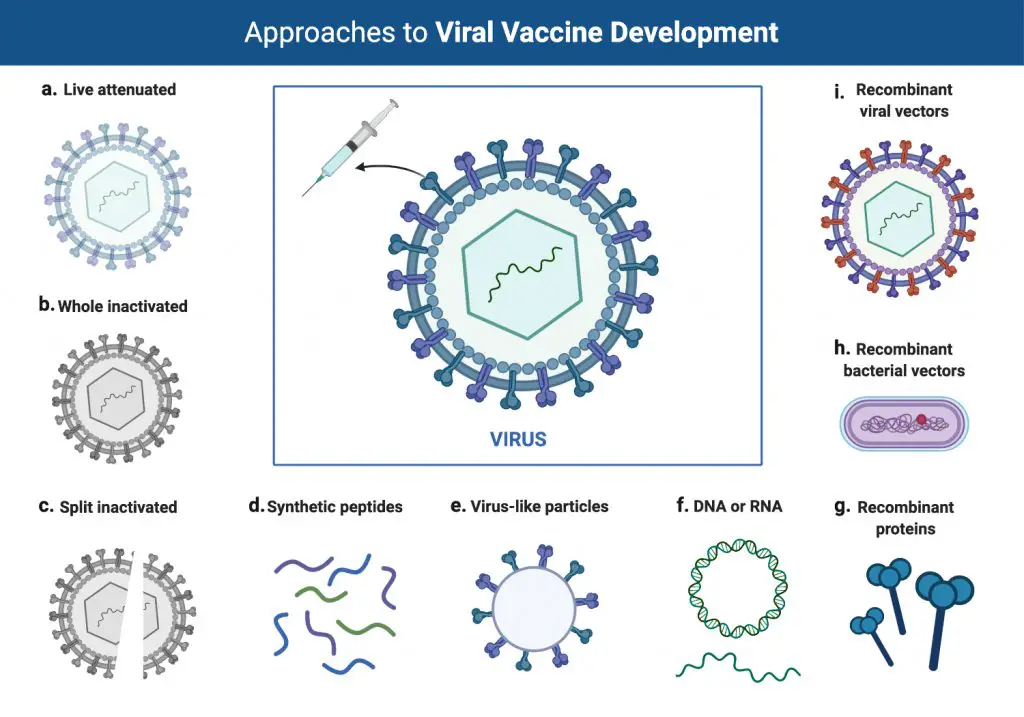
The development of a vaccine is a long process. First, we need to have enough knowledge of pathogens. Second, we need clinical trials to make sure the vaccine is safe. Third, we need to have reliable facilities to produce the vaccine in large quantities. Due to these reasons, the vaccine for COVID-19 may not be available in a short period of time.
The good news is our biotechnology had a tremendous advance in the past decade and several new techniques may make the vaccine ready much faster than before. First, our scientists around the world responded very quickly and successfully isolate the COVID-19 viruses not long after the disease was discovered. Then, they revealed the genome sequence (or genetic codes) and protein structures of COVID-19, both are essential information for designing a vaccine, at unbelievable fast speed. Several pharmaceutical companies have already geared up their research to test vaccines for COVID-19.
Some new techniques may also fundamentally change the traditional way to develop a vaccine. For example, the synthetic RNA vaccination from Moderna Inc, which can be injected into patients to help them create their own therapies, may largely accelerate the development of the COVID-19 vaccine.
11. Can antibiotics or Tamiflu cure COVID-19?
There is no antibiotic to treat COVID-19. Antibiotics are designed for bacterial infections, not viral ones. Tamiflu is an antiviral medication used to treat and prevent flu (influenza A and influenza B viruses). Tamiflu is designed to block an enzyme that flu viruses need to escape from infected cells. Since coronaviruses do so in a different way, Tamiflu may not work for COVID-19 treatment. Some cases show positive results when used Tamiflu in some COVID-19 patients; however, we are still don’t know enough about this disease.
12. Is there other hope on the treatment of COVID-19?
Our scientists around the world keep trying all the methods they can think of to treat COVID-19. For example, a patient who has recovered from COVID-19 infection still have antibodies in their blood (see Adaptive immunity). Scientists from Johns Hopkins Medical School recently found that these antibodies can boost the immunity of newly infected patients and those at risk of contracting the disease. In fact, we know this concept for almost a century, and the Snake antivenom (which is antibodies produced in horses to neutralize snake bites) is the most well-known example.
Although the patients’ serum could be an effective medication for COVID-19, it is almost impossible to obtain the serum in large quantities in a short period of time. These patients who have recovered from COVID-19 need to be healthy and free of other diseases before they can donate their blood. The amount of blood each person can donate is also limited. Prevention of viral spreading, anti-viral drugs, and vaccines still have the highest priority when we face COVID-19.
13. Can we see COVID-19 under a microscope?
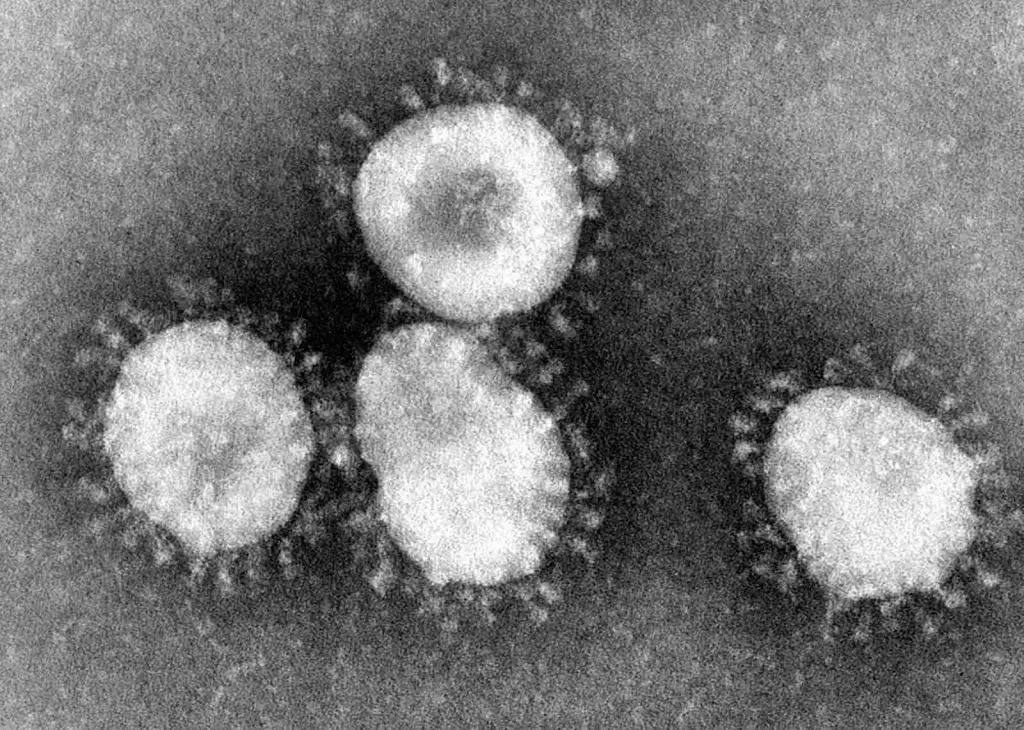
The quick answer is No with an optical microscope, and Yes with an electron microscope.
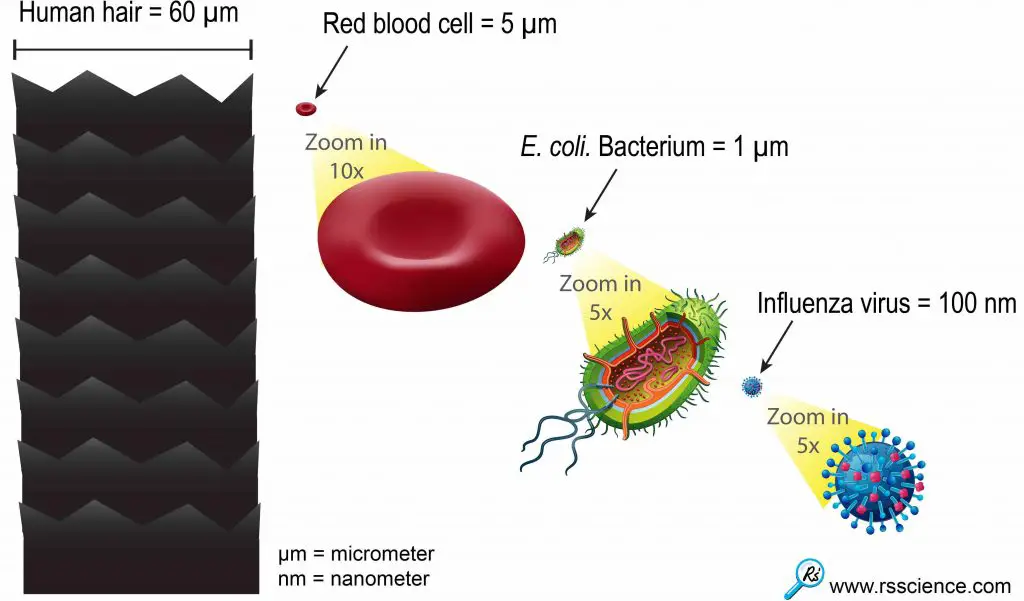
The average sizes of human viruses are around 100 nanometers (1 meter = 1,000 millimeters = 1,000,000 micrometers = 1,000,000,000 nanometer!). A coronavirus is 600 times smaller than the diameter of human hair and 10 times smaller than a bacterium. This scale is outside the limit that typical optical microscopes can see.
We wrote an article about “can you see viruses under a microscope“. We discussed why the optical microscope can not see viruses and why an electron microscope can be used to see viruses. We also include the electron microscopic images of different human viruses.
In order to see things that small, we need an electron microscope. The pictures of COVID-19 that you saw on the news are electron microscopic images.
Coronaviruses have a halo or crown-like (corona) appearance. The new virus, COVID-19, is one kind of coronaviruses. Original electron microscopic images are always black-and-white. The colors are artificially painted for better visualization. Credit: CDC.
14. How do we diagnose COVID-19?
Since COVID-19 viruses are too small to see, we use indirect ways to diagnose COVID-19. One way is based on patients’ symptoms and their chest X-ray/CT scan. However, many symptoms are similar between COVID-19 and flu, so we need more precise methods, called the molecular diagnosis.
The fingerprints of COVID-19 viruses that can confidently identify the origins of infection are their genetic materials, RNA. Since our scientists have already isolated the COVID-19 viruses and interpret their genetic codes, we can design a probe that only recognizes RNA codes from COVID-19 but not from other viruses. Using a technique called Real-Time PCR (quantitative PCR) test, hospitals can screen the specimens from patients to see if COVID-19 RNA is present.
Real-Time PCR test is precise but time-consuming (typically more than 4 hrs) because it involves many steps and expensive equipment in a laboratory. Is there any other way for a faster diagnosis? Scientists are now testing antibody-based diagnosis for COVID-19. This antibody-based diagnosis works exactly like the pregnancy test. The tests consist of strips of paper that are coated with antibodies that bind to COVID-19. The patient’s specimen is added to a solution containing a second antibody which also binds to COVID-19 and is attached to tiny gold particles. The test strip is then dipped in this solution. If the COVID-19 is present, it attaches to the antibodies on the paper strip as well as the gold-bound antibodies, and a colored spot appears on the strip within 20 minutes.
A fancy tool called CRISPR can also use to diagnose COVID-19. CRISPR is a system that we learned from bacteria and modified for gene editing. CRISPR has a huge promise to cure many diseases caused by genetic mutations, like hemophilia and cystic fibrosis. CRISPR can efficiently screen every genetic material that it encounters and find out a particular genetic code sequence. A group of scientists from the Broad Institute (Cambridge, Massachusetts) has used this concept to design a CRISPR test for COVID-19.
15. How can we prevent the infection of COVID-19?
Before we have a vaccine, the best way to prevent COVID-19 is to avoid exposure to the viruses. We know the viruses spread mainly from person-to-person through respiratory droplets produced when an infected person coughs or sneezes. Please take these steps to protect yourself and others:

For more detail, see the CDC website: https://www.cdc.gov/coronavirus/2019-ncov/prepare/prevention.html
*Be respectful of others who wear face masks
You may see people wearing face masks. Although CDC does not recommend widespread use of face masks for asymptomatic people outside clinical settings, please remember that it is a social norm in many countries to wear a face mask during cold, flu and allergy season. Do not assume that a person wearing a face mask is infectious, or that they should be avoided. Treating all members of our community with respect and consideration is as important now as at any other time.
Taiwan is one of a few countries that contain the spread of the virus. One of the reasons is that everyone is very serious about the outbreak of COVID-19 and wears a face mask when going out. The government ensures that all residents have access to masks amid panic buying so they roll out “Name-based rationing system for purchases of masks”. Therefore, I would argue that wearing a face mask is protecting yourself and others.
16. Why washing hands with soap and water is so important right now?
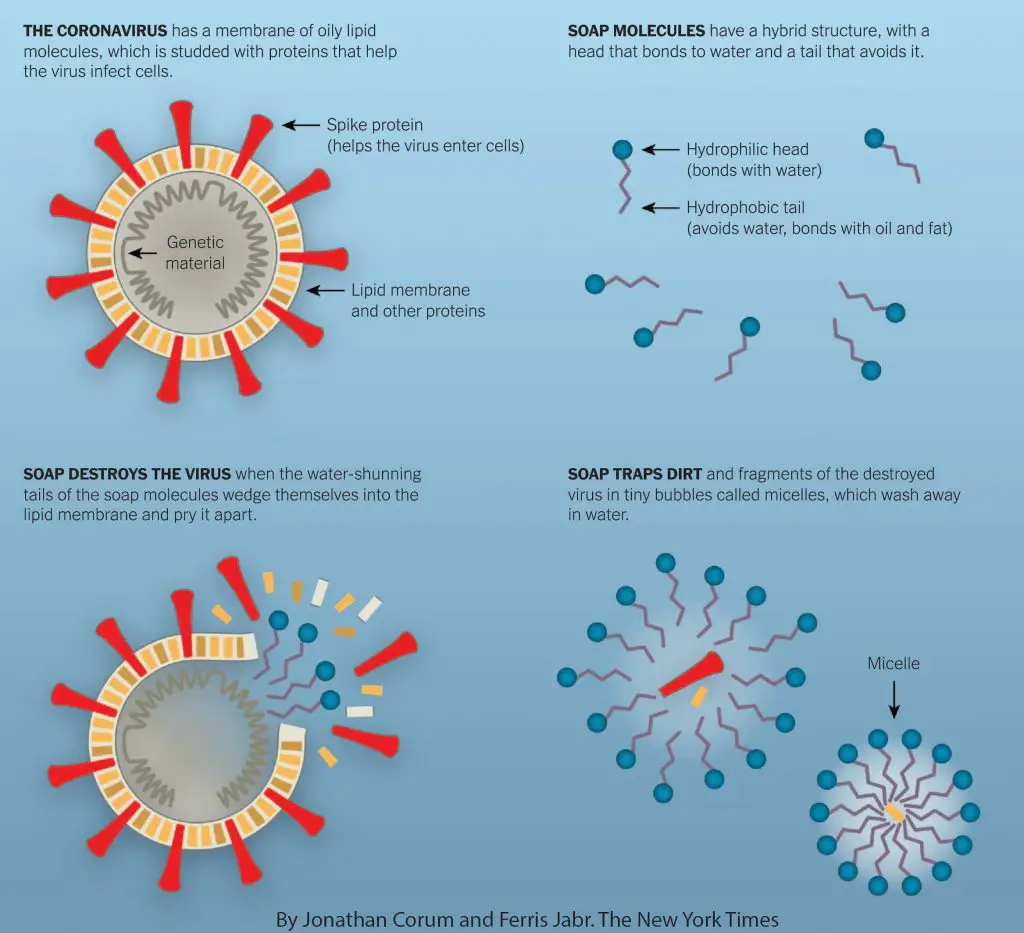
People typically think of soap as gentle and soothing, but from the perspective of microorganisms, it is often extremely destructive. Washing hands with soap and water is sufficient to rupture and kill many types of bacteria and viruses, including the COVID-19 virus that is currently circling the globe. Why? A virus has its genetic material packed in an oily lipid envelope. The soap molecule has a hybrid structure that can easily disrupt the virus’s lipid envelop.
17. Where does COVID-19 come from?
Scientists now are still looking for the origins of COVID-19 by studying the virus’s genetic material. COVID-19 virus has RNA as its genetic material. RNA and DNA are nucleic acids that can store the genetic information in a code system (ATGC for DNA and AUGC for RNA). By sequencing the virus’s RNA molecules, we can know the entire genetic codes (or genome) of this particular virus.
In the most recent study, by comparing the genomes of COVID-19 and related coronaviruses, scientists found that COVID-19 virus has a unique spike protein (the protein which viruses use to invade human cells). This unique spike protein is a result of mutation. Now, they are figuring out when this mutation happened.
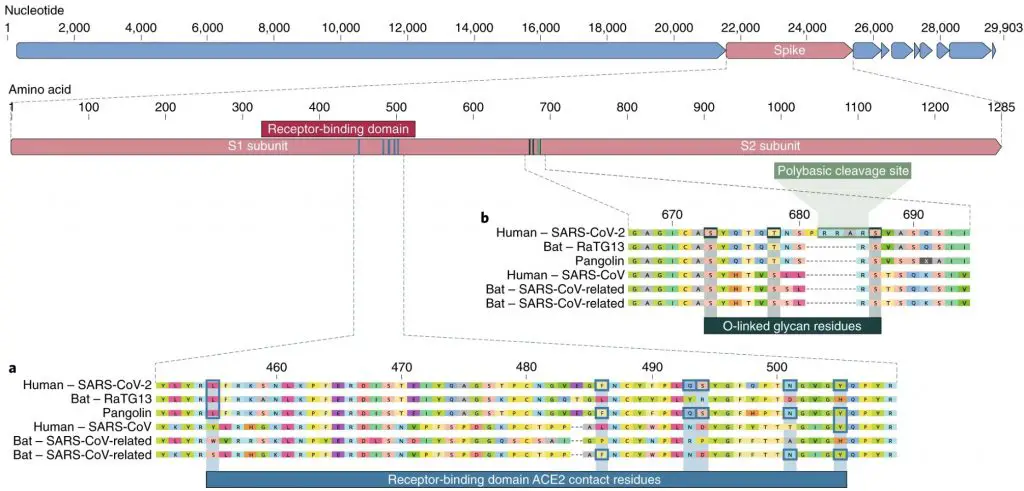
Genome comparison between COVID-19 and related coronaviruses to highlight the mutation in its spike protein. Original article: “The proximal origin of SARS-CoV-2” Nature Medicine (2020). Published: 17 March 2020. https://www.nature.com/articles/s41591-020-0820-9#citeas
Related posts
Can You See Viruses Under a Microscope?
What Living Things You Can See Under a Light Microscope?