This article covers
What are white blood cells – an overview
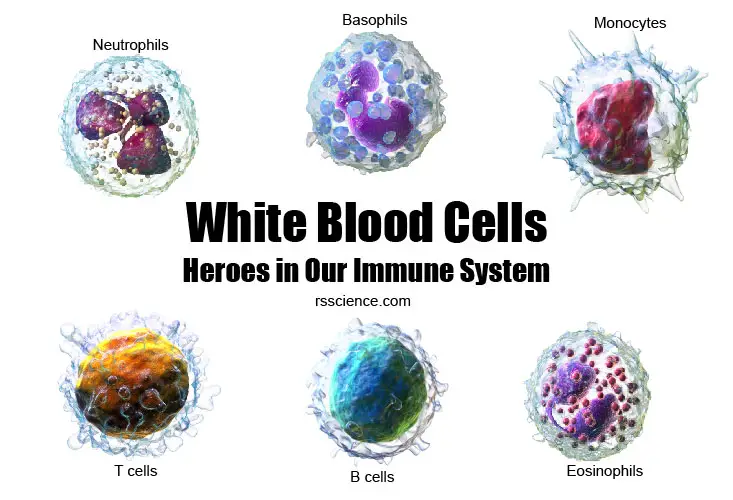
White blood cells (WBCs, also called leukocytes) are a critical part of our body’s immune system. They help the body fight against infection (both bacteria and virus) and other diseases (like cancer). In this article, we will go through the basic biology of white blood cells. You will learn about different types of WBCs and their functions. I will also show you how they look like under the microscope. Are you ready?
[In this video] See the most abundant type of white blood cells – neutrophils – in action.
Circulation system – Heart, Blood vessels, Blood, and Blood cells
In brief, the circulation system transport nutrients, oxygen, and waste to and from the cells in the body to provide nutrients. It also helps in fighting diseases, stabilizing body temperature, and maintaining homeostasis.
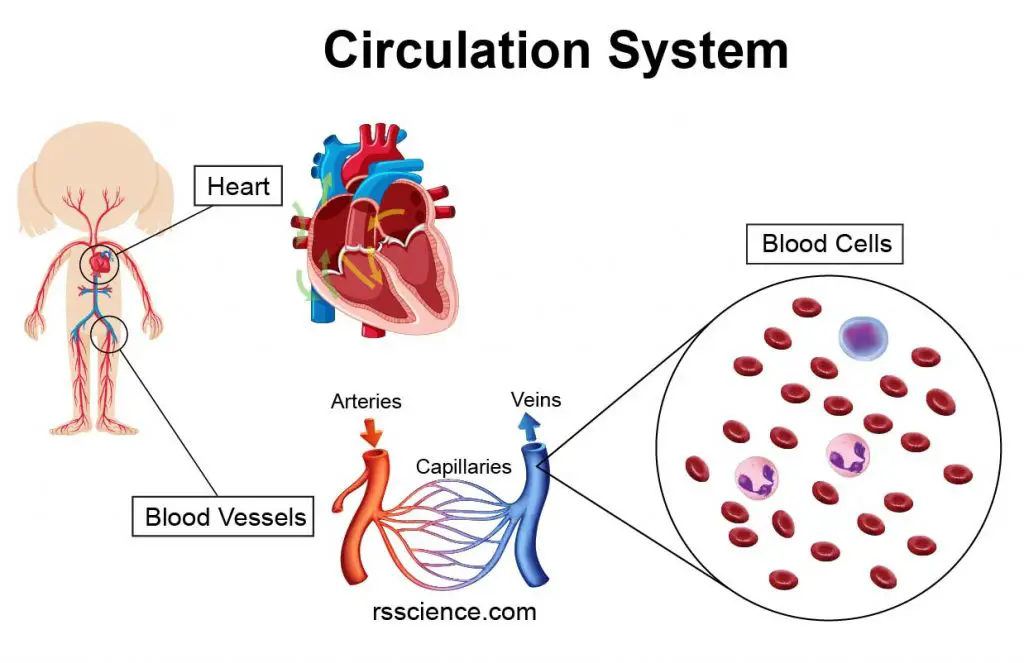
[In this image] The heart, blood vessels, and various blood cells constitute our circulation system.
The essential components of the circulation system include the heart, blood, and blood vessels. The heart pumps oxygenated blood to the body and recycles deoxygenated blood to the lungs. Blood is carried through the body via blood vessels.
Blood is a body fluid that transports nutrients, oxygen, and metabolic waste products in our bodies. It is composed of blood cells in blood plasma. Plasma, a yellowish fluid, is mostly water and contains various proteins, blood sugar, ions, and carbon dioxide. The average adult has a blood volume of roughly 5 liters.
The blood cells are mainly red blood cells (also called RBCs or erythrocytes), white blood cells, and platelets. By volume, the red blood cells constitute about 45% of whole blood, the plasma about 54% of the blood volume, and white cells about 1% of volume.
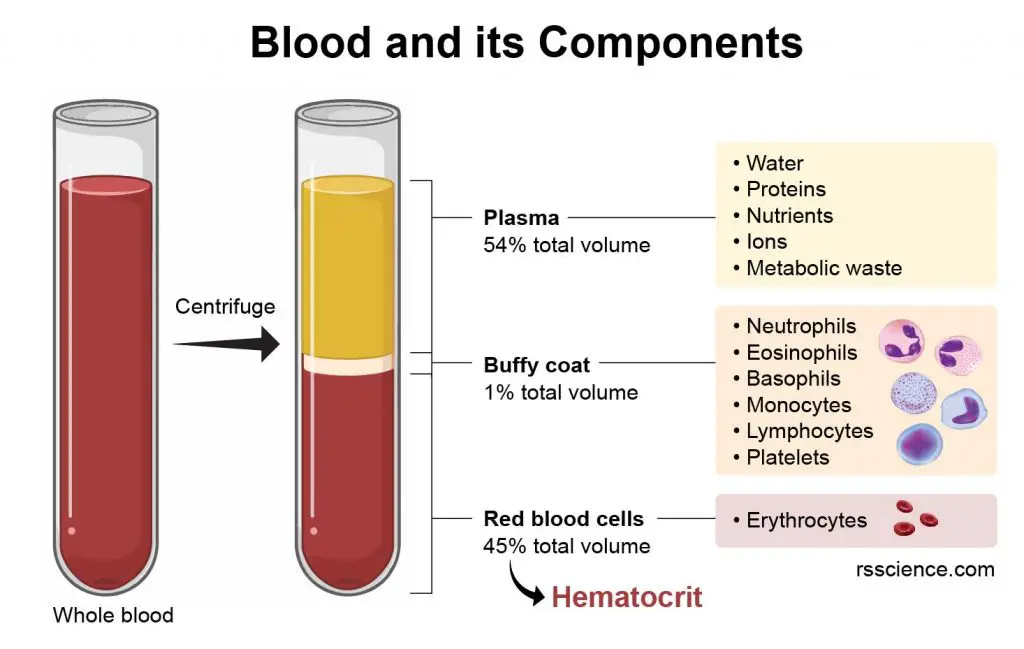
[In this image] Blood contains plasma and blood cells. Their relative amounts can be measured by the packed volume after the centrifugation. Between the plasma and RBCs is a thin layer of the white stuff, called Buffy coat. Buffy coat contains a mixture of various white blood cells and platelets.
Why white blood cells are important?
White blood cells make up approximately 1% of the total blood volume in a healthy adult, making them substantially less numerous than the RBCs. However, this 1% of the blood makes a huge difference to health, because our immunity depends on it. The number of WBCs is often an indicator of disease. For example, if the body has a bacterial infection, the WBC count can significantly increase in order to fight bacteria.
[In this video] Large cells moving along the blood vessels are leukocytes.
When infection occurs, leukocytes transmigrate through the blood vessel walls and move to the infected site.
Leukocytes play a central role in protecting our body from various microorganisms (i.e., bacteria, yeasts, and protozoa), viruses, and parasites (i.e., helminths and ectoparasites). Moreover, they are also involved in the elimination of cancer cells. Recently, scientists found that even in a sterile wound (like stroke or heart attack), tissue repair and regeneration also require certain types of white blood cells.
In some cases, however, leukocytes may be the cause of diseases once they are out of control. One example is allergic reactions when our immune system overreacts to foreign antigens. Another example is autoimmune diseases, in which our immune system attacks our own cells.
Classification of white blood cells
Based on the criteria, there are several ways to classify WBCs:
A. based on the presence of granules and the nucleus shapes
Depending on whether they contain granules or not, the white blood cells can be divided into two main types: granulocytes and agranulocytes.
Neutrophils, eosinophils, and basophils are all granulocytes because of their high content of granular organelles. These granules store special enzymes for their immune functions. These leukocytes also have lobed/segmented nuclei, so-called polymorphonuclear (PMN) leukocytes.
On the other hand, lymphocytes and monocytes are classified as agranulocytes due to the lack of granules. They are also named mononuclear leukocytes due to the nucleus morphology.
B. based on their origins
Hematopoietic stem cells are capable to give rise to all types of blood cells. The differentiation goes through two major lineages: the lymphocytic or the myelocytic lineage. Based on this definition, all granulocytes and monocytes are myeloid cells.
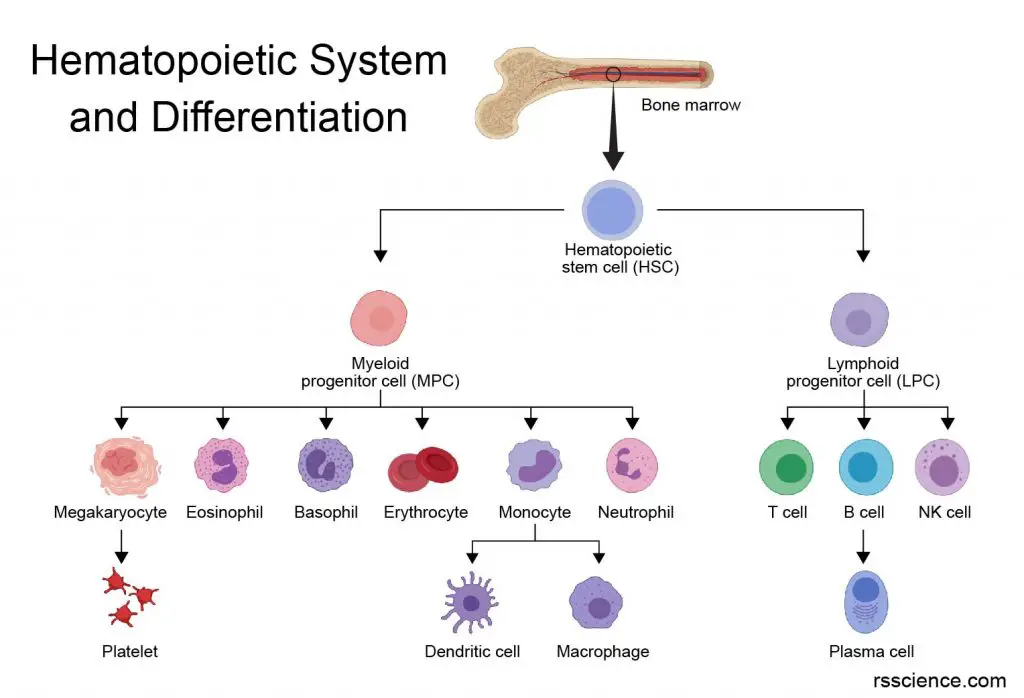
[In this image] The family of the hematopoietic (meaning blood) system is originated from the hematopoietic stem cells in our bone marrow.
C. based on the roles in immune system
Innate immune responses are not specific to a particular pathogen whereas the adaptive immune responses are. The innate immune cells, including granulocytes (neutrophils, eosinophils, and basophils), monocytes (macrophages and dendritic cells), and natural killer (NK) cells, can quickly defend potential invaders. In contrast, B cells and T cells (both are lymphocytes) are adaptive immune cells, which can remember the pathogens encountered before and defend effectively. This is why we need to get vaccines.
D. based on the ability to engulf pathogens
Both monocytes and neutrophils are phagocytic. You can call them professional phagocytes. They can easily engulf entire pathogens by “eating” (or called phagocytosis).
E. based on their locations
Leukocytes are usually referred to as white blood cells circulating in the bloodstream. When they leave the circulation into tissues, they adapt to the tissue environments and change their properties. For example, circulating monocytes become macrophages by increasing their cell size and phagocytic capability in tissues. Mast cells and dendritic cells are also white blood cells residing in tissues.
Types of leukocytes – Characteristics and Functions
In this section, we will go through several types of white blood cells in detail.
| Type | Neutrophil | Eosinophil | Basophil | Monocyte | Lymphocyte |
| Appearance | 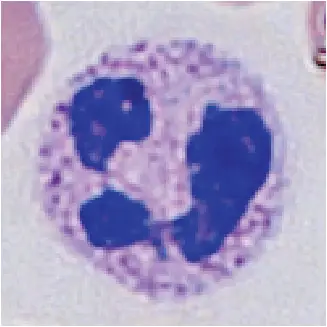 | 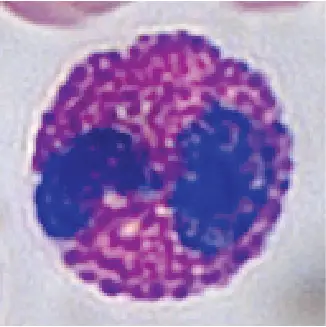 | 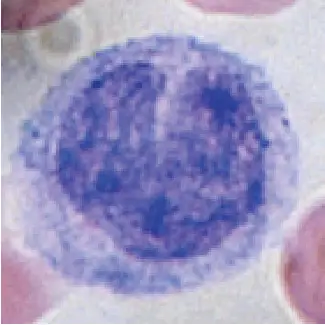 | 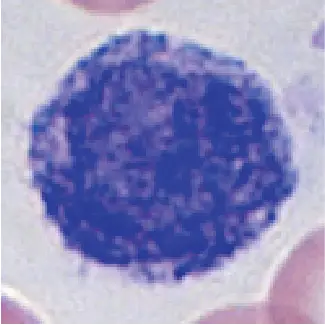 |  |
| Percentage in total WBCs | 65% | 2-4% | 0.5-1% | 2-6% | 20-30% |
| Cell size (diameter) | 10-12 µm | 10-12 µm | 8-10 µm | 12-20 µm | Small: 7-8 µm Large: 10-12 µm |
| Nucleus | 2-5 lobes | 2-3 lobes | 2 lobes | Kidney shaped | Round |
| Granules | Yes | Yes | Yes | No | Only in large lymphocytes |
| Phagocytosis | Yes | Yes | No | Yes | No |
| Main functions | Defense bacteria | – Defense parasites – Modulate allergic inflammatory responses | Release histamine for inflammatory responses | Phagocytosis – Present antigens | T cells – regulate adaptive immunity B cells – produce antibodies NK/T cells – kill virus-infected and tumor cells |
Neutrophils
Neutrophils are the most abundant white blood cells (approximately 65% of the WBCs) which protect us from bacterial infection. Neutrophils have a highly lobed nucleus (between 2-5 lobes) and cytoplasm containing many reddish-purple granules.
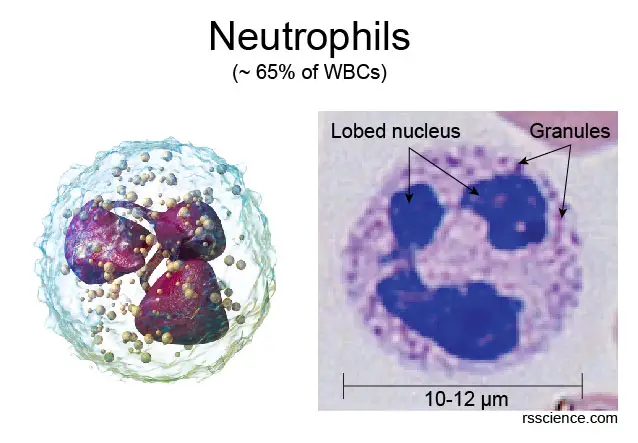
[In this image] Neutrophils are characterized by their segmented nuclei and granules.
Left: 3D rendering of a neutrophil. Right: A human neutrophil imaged from a blood smear with Wright’s stain.
Photo credit: modified from wiki
Neutrophils are the first line of defense. Their weapon is the ability to engulf the whole bacteria by phagocytosis. Neutrophils can break down bacterial cell walls thus killing them by lysozyme in their granules. In addition, they also release proteins known as defensins that bind and destroy the plasma membrane of both fungus and bacteria.
[In this video] Neutrophils chasing bacteria under the microscope.
In the worst-case scenario, neutrophils are willing to sacrifice themselves to contend the infection. The death of neutrophils will release their nuclear DNA, forming a network of extracellular fibers, called neutrophil extracellular traps (NETs). NETs can bind and kill pathogens while minimizing damage to the host cells.
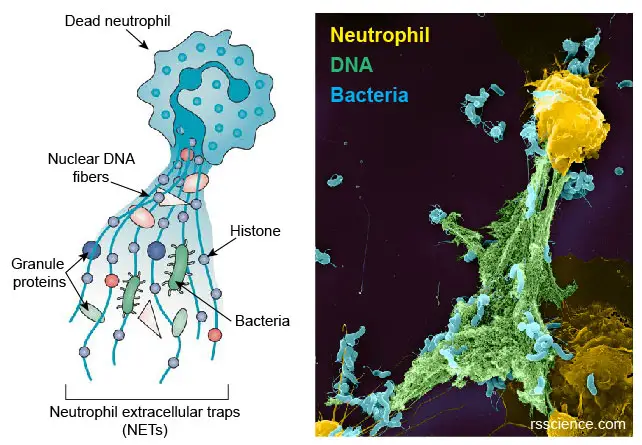
[In this image] Dead neutrophils release nuclear DNA and proteins to form a web (NET) which can trap pathogens.
Left: The diagram showing the compositions of NETs. Right: A colored SEM image showing neutrophils (yellow), DNA fibers (green), and bacteria (blue).
Modified from Daniel C., et.al., Nature Reviews Nephrology, 2019; Thalin C., et. al., Arteriosclerosis, Thrombosis, and Vascular Biology, 2019
Eosinophils
Eosinophils contribute to 2-4 percent of the total white blood cells. Eosinophils have nuclei with 2-3 lobes. Eosinophils get their name due to their acidophilic (acid-loving) cytoplasmic granules, which show high affinity to acidic dye, eosin (for this reason, eosinophils stain much more reddish than other cells). These granules contain many chemical mediators. These mediators are released by a process called degranulation following activation of the eosinophils. Eosinophils are responsible for combating the infection of parasites.
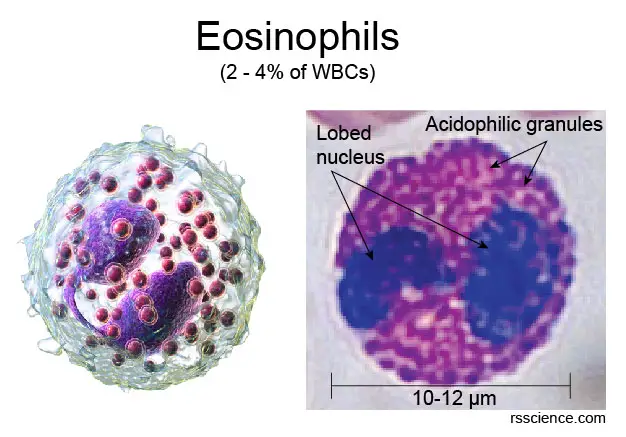
[In this image] “Acid-loving” granules in the cytoplasm of eosinophils are stained heavily by eosin dye, giving them a brick-red appearance.
Photo credit: modified from wiki
Basophils
Basophils are the least common WBCs (only 0.5 to 1%). The name comes from the fact that basophils are basophilic (base-loving), i.e., they are susceptible to staining by basic dye (as a result, basophils look more blueish among WBCs). Basophils have a bi-lobed nucleus.
Basophils are responsible for inflammatory reactions during an immune response. This is achieved by the release of histamine and serotonin that promote inflammation. Basophils also release heparin that inhibits blood clotting. Mast cells share many functional similarities with basophils. However, mast cells stay within tissues.
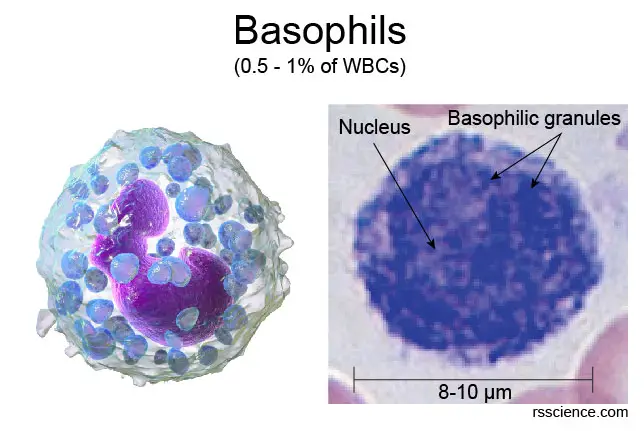
[In this image] Basophilic granules mark basophils with strong blue staining under the microscope.
Photo credit: modified from wiki
Monocytes
Monocytes share the “vacuum cleaner” function of neutrophils, meaning they can engulf (or eat) pathogens by dramatically changing their cell shape like an amoeba (a process called phagocytosis). They make up 2-6 percent of the total white blood cell count and can be recognized by their horseshoe or kidney-shaped nuclei. Monocytes are also larger in size when compared to other leukocytes, measuring between 12 and 20 µm in diameter.
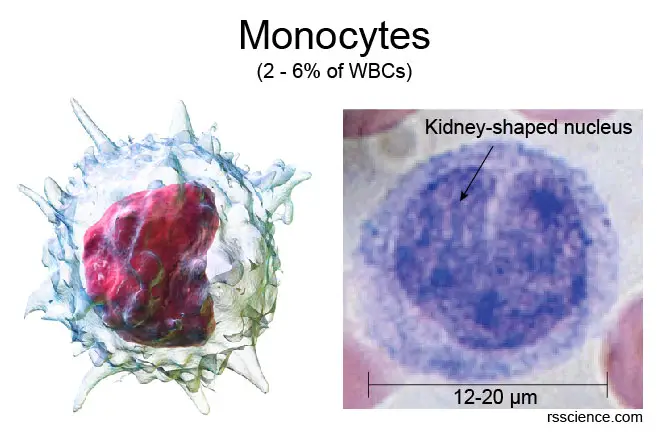
[In this image] Monocytes are characterized by their horseshoe or kidney-shaped nuclei under the microscope.
Photo credit: modified from wiki
Monocytes patrol our body, remove dead cell debris, and attack microorganisms. Monocytes can eventually leave the bloodstream and become macrophages in the tissues, continuing to guard every inch of our body. Both monocytes and macrophages destroy invading pathogens through phagocytosis. At the same time, they also release various chemicals that amplify inflammatory responses and recruit other leukocytes to the affected site.
Macrophages
When monocytes leave the bloodstream, they become macrophages in the tissues. Macrophages patrol for potential pathogens by amoeboid movement, changing their shapes to migrate between cells. They take various forms (with various names) throughout the body. For example, specialized macrophages are called histiocytes, Kupffer cells, alveolar macrophages, and microglia in the skin, liver, lung, and brain, respectively.
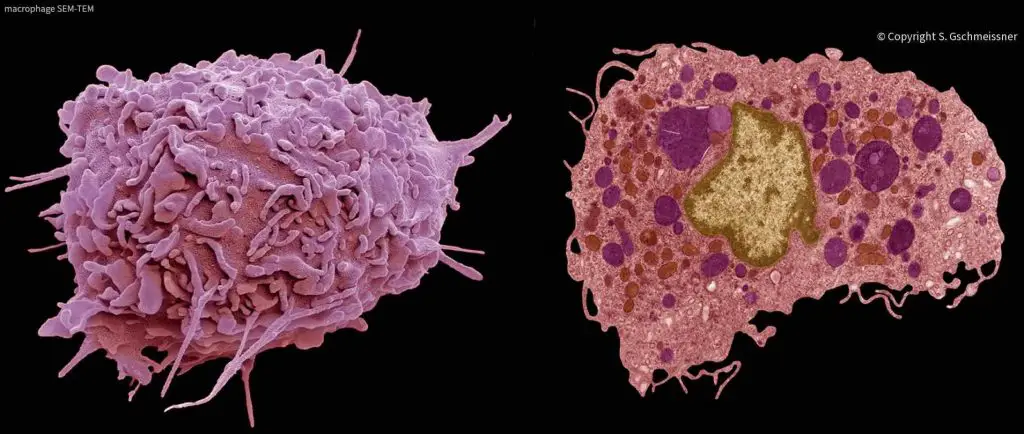
[In this image] SEM (left) and TEM (right) images of macrophages.
Photo credit: Stephen Gschmeissner
Macrophages are professional phagocytes, which engulf and digest anything that does not have, on its surface, proteins that are specific to healthy body cells, including cancer cells, microbes, cellular debris, foreign substances, etc. Macrophages also tell T cells if anything (like pathogens) needed to pay attention to. This process is called “antigen-presenting”, which can activate T cells and adaptive immunity.
[In this video] See how macrophages eat bacteria under the microscope.
Dendritic cells
Dendritic cells (DCs) are another type of professional antigen-presenting cells that link innate and adaptive immunity. Parts of DCs come from monocytes as well.
Dendritic cells are present in tissues that are in contact with the external environment, such as the skin and the inner lining of the nose, lungs, stomach, and intestines. The name came from the cell morphology of their ‘tree-like’ or dendritic shapes. DCs use these cellular protrusions to extend their guard ranges. Once they find pathogens, they will migrate to the lymph nodes where they interact with T cells and B cells to initiate and shape the adaptive immune response.
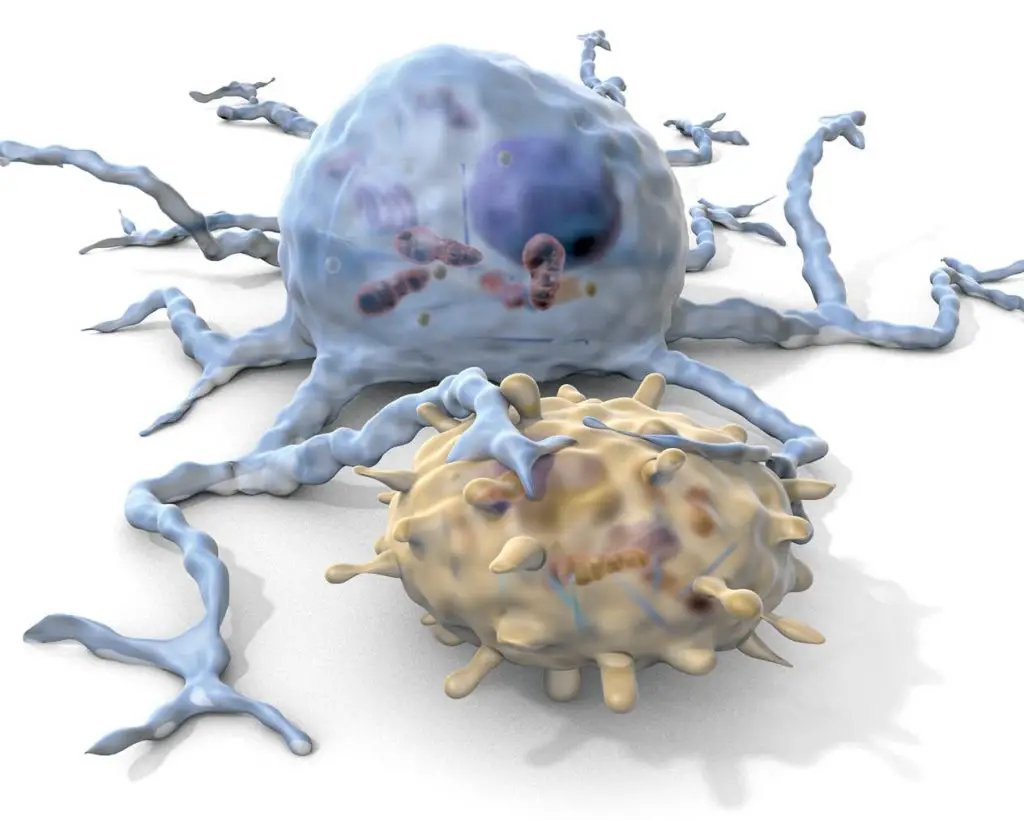
[In this image] A dendritic cell (blue) engages a T cell (yellow).
Photo credit: Mueller KL, Science, 2014
Lymphocytes
Lymphocytes include T cells, B cells, and Natural killer (NK) cells. They are the main type of cells found in lymph, which prompted the name. They make up 20-30 percent of the total white blood cell count and vary significantly in size. T cells and B cells are the major cellular components of the adaptive immune response. They can identify invaders and generate antibodies to destroy these pathogens.
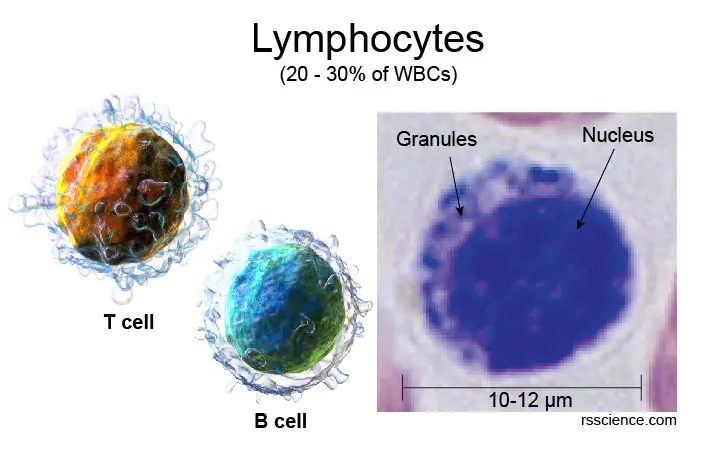
[In this image] Lymphocytes have round nuclei which occupy a significant portion of the cells.
The size of lymphocytes varies upon their degree of maturation. Small lymphocytes range from 7–10 µm in diameter. Large granular lymphocytes range from 10–12 µm in diameter and contain more cytoplasm and scattered granules.
T Cells
T cells have the T-cell receptors (TCR) on their cell surface and play a central role in the adaptive immune response. Developing T cells have to migrate to the thymus gland to mature. This is why the name “T” came from.
T cells can be divided into two major subtypes: CD8+ “killer” and CD4+ “helper” T cells. CD8+ “killer” T cells are cytotoxic – this means that they are able to directly kill virus-infected cells, as well as cancer cells. On the other hand, the CD4+ “helper” T cells guide the activation of B cells, which can kick-start the adaptive immune response. CD4+ T cells are the major victims of HIV infection.
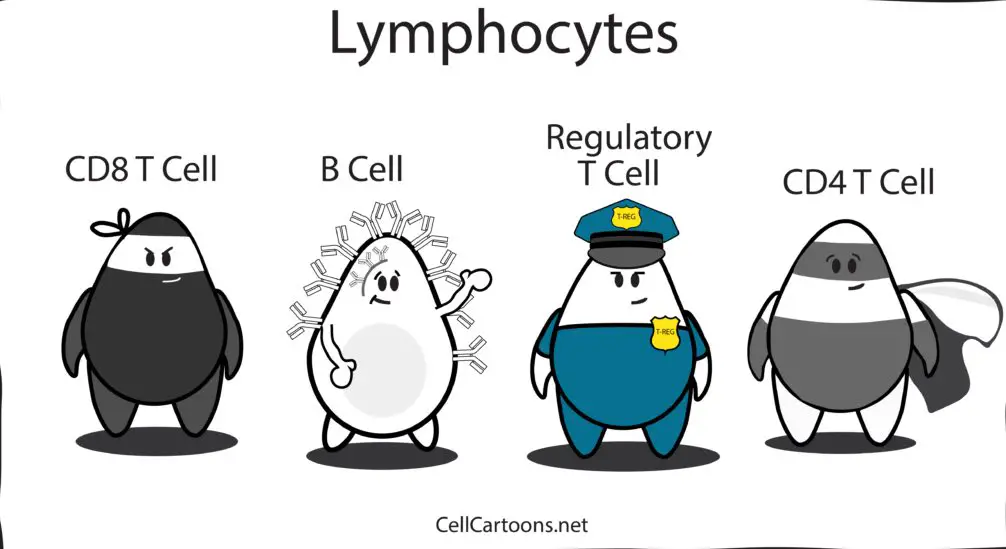
Photo credit: Cell Cartoons
More recently, small populations of T cells, called Regulatory T cells (Treg), were identified by immunologists. Regulatory T cells can suppress the immune response and provide tolerance. This prevents immune cells from inappropriately reacting against ones’ own cells, which can cause autoimmune diseases.
B cells
B cells function in adaptive immunity by producing antibodies that neutralize foreign objects such as bacteria and viruses. Adaptive immunity creates immunological memory after an initial response to a specific pathogen and leads to an enhanced response to future encounters with the same pathogen. This process is highly controlled by the interaction between B cells, T cells, and other immune cells. Activated B cells will become plasma cells with enhanced capability to produce large quantities of antibodies.
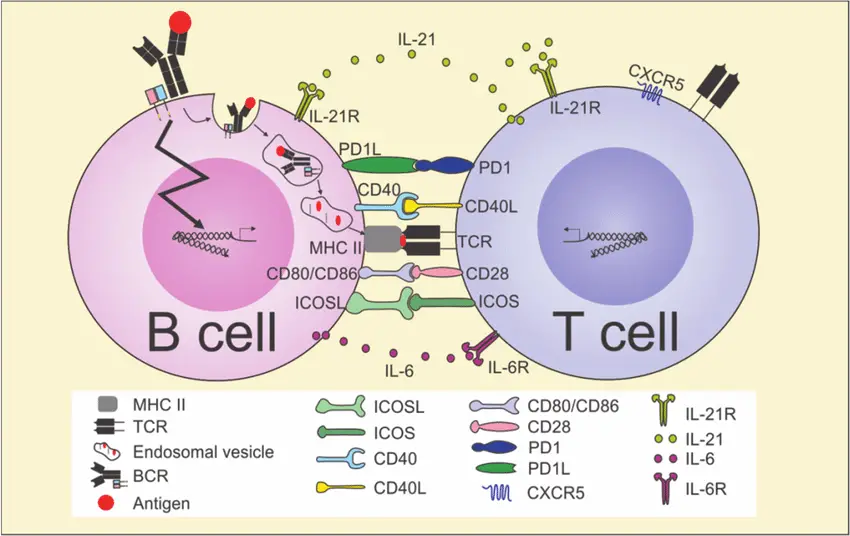
[In this image] There is a complicated communication between T cells and B cells to ensure the proper performance of the immune system.
Photo credit: ResearchGate
A vaccine is a way to introduce this kind of immune memory even before we face the real infection. That is why we need to have several vaccinations in order to prevent deadly diseases, like flu, polio, and measles.
Natural killer cells
Natural killer cells, also known as NK cells, are a type of cytotoxic lymphocytes but belong to the innate immune system. The role of NK cells is analogous to that of killer T cells. NK cells provide rapid responses to virus-infected cells. NK cells are heavily studied now for their potential to kill cancer cells.
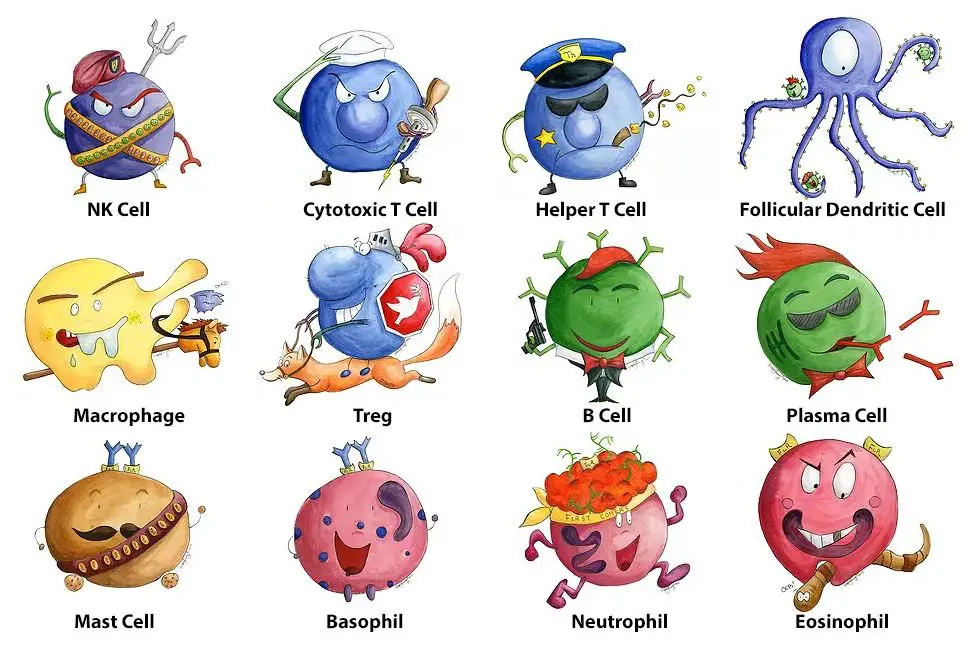
Photo credit: Pinterest
Which organ produces white blood cells?
White blood cells are made in the bone marrow. They are stored in your blood, lymph tissues, and spleen. Because some white blood cells including neutrophils have a lifetime less than a day, your bone marrow is always making them.
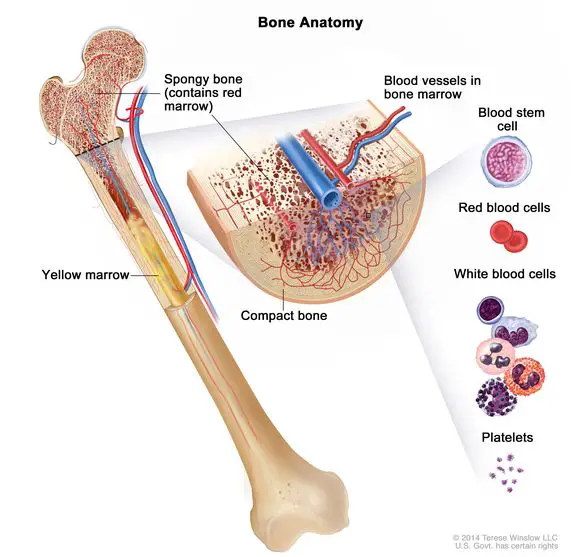
[In this image] All blood cells (WBCs, RBCs, and platelets) are produced by blood-forming cells, called hematopoietic stem cells, in the bone marrow.
Photo credit: NIH
Look at white blood cells under a microscope
Blood smear
If you just add a drop of blood on a microscopic slide, the specimen will be too “thick” (too many red blood cells) to observe. The best solution is to prepare a “Blood Smear”.
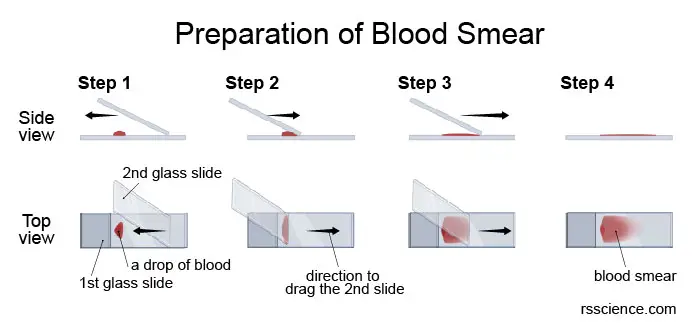
[In this image] Microscopic examination of whole blood begins with the preparation of a smear:
(1) A small drop of blood is placed at one end of a glass slide.
(2) Draw across the drop at an angle with the edge of a second slide. The capillary force will spread the drop along the edge.
(3) Push the second slide smoothly to the opposite end of the first slide, spreading the drop across the slide to make the smear.
(4) The blood smear is thicker at one end but becomes thinner to the opposite end.
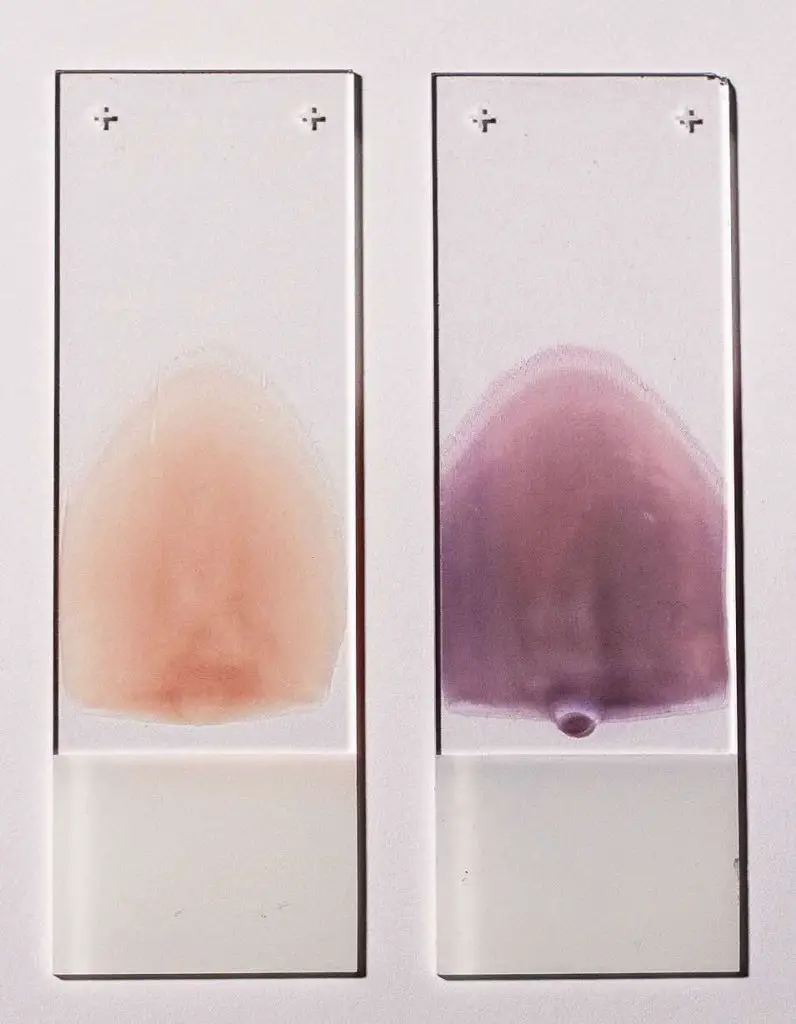
[In this image] Two blood smears suitable for characterization of blood cells.
Left smear is unstained, right smear is stained with Wright-Giemsa stain.
Photo credit: wiki
Wright’s stain
After the smear is air-dried, it can be stained by Wright’s stain. Wright’s stain is the most common technique to stain blood specimens. It contains red (eosin) and blue (methylene blue) dyes that are acidophilic (‘acid-loving’) and basophilic (‘alkaline-loving’), respectively. Eosin stains cytoplasm and acidophilic granules. Methylene blue stains basophilic granules and nuclei by binding to DNA.
A modified version of Wright’s stain called Wright-Giemsa staining (composed of methylene blue, azure B, and eosin) is commonly used in hematology and bacteriology. Blood smear stained by Wright-Giemsa method will show:
| Erythrocytes | pink |
| Platelets | pale pink |
| Neutrophil granules | purple-pink |
| Eosinophil granules | red |
| Basophil granules | blue |
| Lymphocyte granules | red-purple |
| Lymphocyte cytoplasm | sky blue |
| Nuclei | dark blue |
Blood cells under the microscope
If the blood film is properly prepared and stained, we should be able to easily see individual cells under a bright-field microscope. You can use the characteristics we mentioned above and the examples below to identify each type of leukocytes.
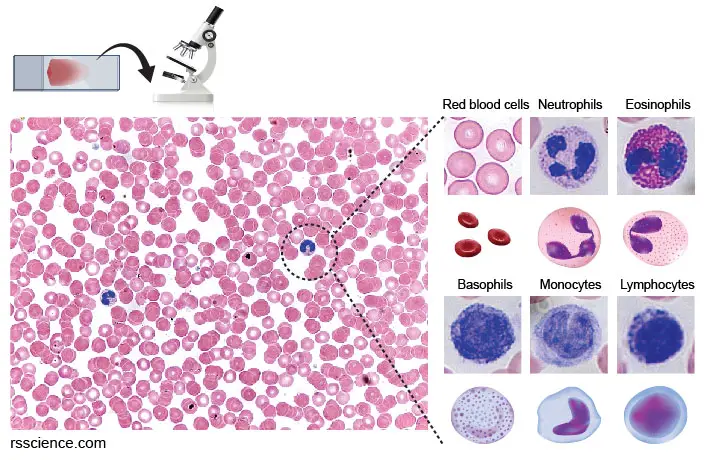
[In this image] Blood smear with Wright-Giemsa stains.
You can look at these blood cells under a bright-field microscope. You can see cells under a low (20x) magnification. However, if you really want to distinguish the types of WBCs by their nucleus and granule morphology, you probably have to go higher to 63x-100x.
The most abundant cells in the blood are red blood cells (RBCs). Human RBCs don’t have nuclei and look like a dish. They are red in color because of the high amount of hemoglobin (the protein that can carry oxygen) in their cytoplasm. You can also see several types of white blood cells at a much lower frequency.
White blood cell count
By examining the blood smear, an experienced hematologist can tell if something is wrong in the blood by looking for any irregular cell morphology or abnormal frequency of certain cell types. Now, regular blood examination is done by automated differential blood count machines for less time-consuming and less expensive.
For healthy individuals, the normal white blood cell count ranges between 5,000 and 10,000 cells per microliter of blood for men and 4,500 and 11,000 for women.
Problems affecting white blood cells
When your white blood cell count is low, you are at great risk for infection. Weak immunity is often caused by illnesses such as HIV/AIDS or by cancer treatment (chemotherapy or radiation therapy).
Too many white blood cells also indicate something wrong in your body. A higher-than-normal white blood cell count usually means you have some type of infection. Blood cancers including leukemia and lymphoma can cause uncontrolled growth of an abnormal type of blood cells in the bone marrow.
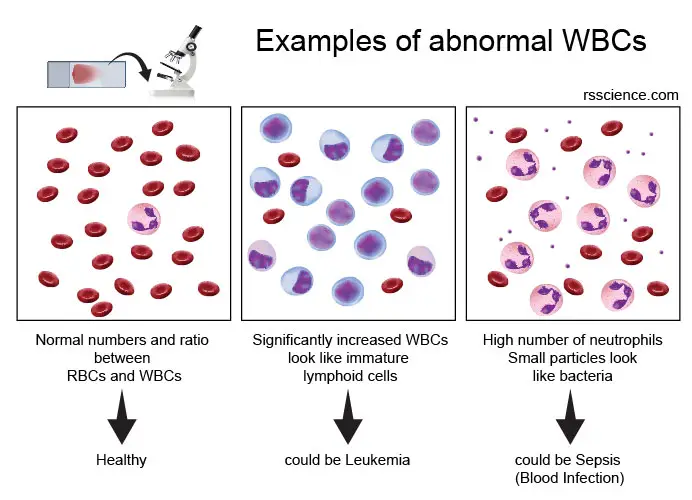
[In this image] Because many diseases will reflect on the dysregulation of blood cells, a blood test is routinely performed in the hospitals for disease diagnosis. Here are examples. An experienced hematologist can have a clue of what is wrong in your body by examining your blood cells based on the complete blood count (CBC) or blood smear.